The Health and Care Act 2022 has cleared away Clinical Commissioning Groups (CCGs) in England and transferred their funding and commissioning powers to 42 Integrated Care Systems (ICSs).
But what has prompted this far-reaching change – and what will it mean in practice?
We attempt to answer the most-asked questions about the introduction of ICSs and reveal what the healthcare landscape will look like under the new system.
Why have CCGs been dissolved?
A decade ago, CCGs were introduced as a partial replacement for Primary Care Trusts (PCTs). CCGs were founded on the belief that GPs were best placed to decide how to spend the money allocated to them to provide positive health outcomes for their patients.
However, concerns over the ability of GPs to influence procurement within a CCG, plus fears around bureaucracy, resource allocation, local accountability, and the ability to provide integrated care, led to their replacement in July 2022 by new regional teams in charge of commissioning, organised into 42 ICSs.
If nothing more, the consolidation of 106 CCGs to 42 ICSs (there were originally over +200 CCGs when they were first introduced back in 2013) presents an opportunity for further efficiencies, achieving enhanced value for money through economies of scale.
What is an ICS and how does it operate?
There are 42 ICSs in England. They vary in size and scope, but all aim to provide more joined-up care for patients. This can mean anything from ensuring that all the different parts of a patient’s care are coordinated, to providing a single point of contact for patients who need help navigating the health and social care system.
Each ICS is expected to establish and improve partnerships among health care partners, handle disparities across populations, and improve outcomes and accessibility whilst enhancing productivity and cost-effectiveness.
Budgets for ICSs are granted directly by NHS England and managed by an Integrated Care Board (ICB), a statutory body responsible for overseeing an ICS.
ICB’s distribute their funding amongst partner organisations to provide core NHS services, with access to funding tied to an ICSs overall performance. There is a strict limit on funding, so ICS boards will need to closely monitor service use and quality.
In addition, each ICS also contains an Integrated Care Partnership (ICP). ICPs have a broader focus, including public health, mental health services, social care and the wellbeing of their communities, and are required to produce an Integrated Care Strategy for the area in which they operate. Representatives from both the local authority/s and the ICB will be statutory members of the ICP.
What are the biggest challenges facing ICSs in England?
The transition from a system that provides treatment for acute conditions in hospitals, to one that provides care for patients in their local communities will be driven by ICSs.
ICSs will need to find ways to improve the coordination and organisation of different health service professionals, which can lead to fragmentation of care and poor patient outcomes, and ensure they have the right mix of providers to provide the best care for local people.
How will service providers work with an ICS?
The aim of this change is to improve patient care by ensuring that all providers embrace common objectives and that patients have a single point of contact for all their care needs. It is also hoped that this change will lead to cost savings as providers will be able to work more efficiently together.
As a result, a key challenge for service providers is to ensure that they are working towards the same goals and share a common vision for integrated care. They also need to put in place robust systems so that patient data can be shared securely between organisations.
Another potential challenge will be making sure that patients receive the right care at the right time. This requires close coordination between providers, as well as effective communication with patients and their families.
There are also concerns that the lack of standardisation between how different ICSs operate could make it difficult for patients to move between them.
How will procurement change under an ICS?
The move from 106 CCGs in England to 42 ICSs will consolidate spend in in doing so, change the healthcare procurement landscape.
Using data from Oxygen’s Insights Spend we have overlaid the spend by CCGs for 2021-2022 onto the new ICS structure, which indicates that almost 43% of spend will be concentrated into the hands of the top 10 ICSs:
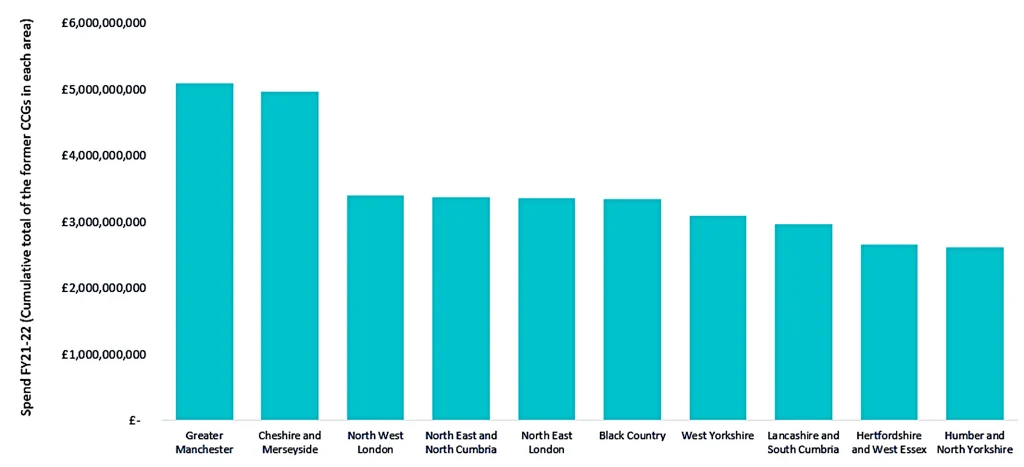
In theory, ICSs can improve care co-ordination whilst also reducing costs. To deliver this, ICSs’ will require new, more collaborative procurement arrangements between providers.
Procurement teams within an ICS may be required to develop new skills and relationships to buy goods and services collaboratively across different organizations, whilst still ensuring that spending is efficient and meets the needs of patients and staff.
The joined-up approach demanded by the breadth of care provision overseen by ICSs will also place a strong emphasis on using data to drive decision-making.
Conversely, providers will need to be able to track and report on spending and performance data to demonstrate value for money.
Oxygen’s Insights team will continue to track healthcare spend under the new system through Insights Spend, and report on how the introduction of ICSs changes the shape of healthcare provision.